Medicare claim life cycle
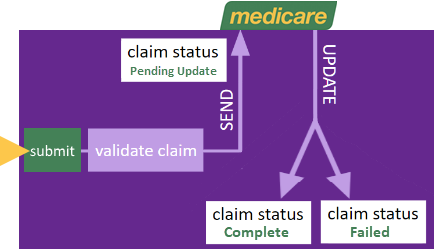
When you submit a Bulk Bill or Patient Paid Medicare claim from an invoice it is first validated by Case Manager to ensure that it contains the required information.
If it does not pass validation the problem(s) are displayed and the process goes no further. You should correct the claim details and re-submit the claim.
When the claim passes validation it is given Pending Update status and sent to Medicare.
With time Medicare either accepts and pays the claim or rejects it and give reason(s). Case Manager can monitor this process and when it has completed the claim outcome details are displayed. The claim is given a status of Complete or Failed as appropriate.
Pending claims are not updated automatically at Case Manager. You can check for updates any time to find out whether, when and how Medicare has resolved them.
Payment transactions
When Bulk Bill claims have been successfully completed you can create a payment transaction, as you would for any other direct deposit.
When the patient pays you would create a payment transaction on the spot, as you would for any other kind of payment.
Claim status
A claim submitted to Medicare has a status of Pending Update.
There are two possible outcomes:
- The claim is accepted and Medicare pays the claim.
- The claim is rejected by Medicare.
In Case Manager the claim will be given Complete status and the finalisation date, amount and payment run are displayed.
In Case Manager the claim will be given Failed status and the error code and any additional notes received from Medicare are displayed.
View claim details
To view a claim select its invoice and click Medicare Claim, at the bottom of the invoice cost details:
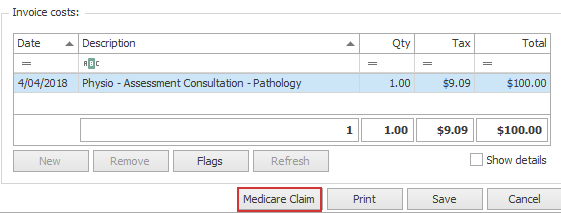
Claim details are displayed including:
- the type of claim,
- the submission date,
- the claim Id
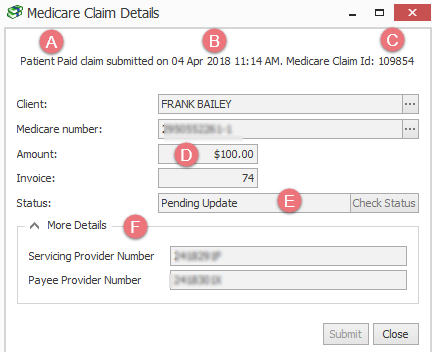
- the claim amount
- the claim status
- The More Details area contains further details, depending on the claim type.
- When the claim has been accepted by Medicare you will also see the benefit paid and the payment run.
- When the claim has been rejected by Medicare you will also see the error code and any extra feedback in the Assessor notes.
Check for updates to claims
Claims with Pending Update status are not updated automatically in Case Manager when Medicare makes a decision to either accept or rejected them. Instead you need to request that Case Manager checks for any updates to pending claims.
Multiple claims
To check for a updates to all claims with Pending Update status, click Check for Status Updates at the top of the Medicare claim grid:
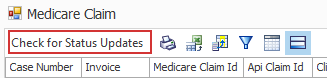
You will need to close the current grid and re-open it again in order to refresh the list.
One claim
To check for an update to one claim locate the invoice, click Medicare Claim to view the claim details and click Check Status.
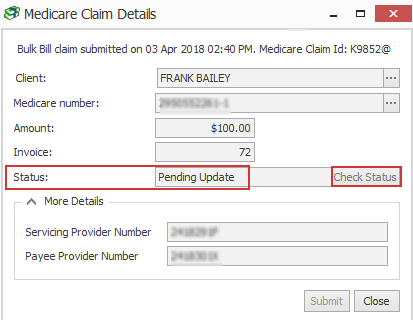
If there's been an update the claim status will change to Complete or Failed and the claim details are updated.
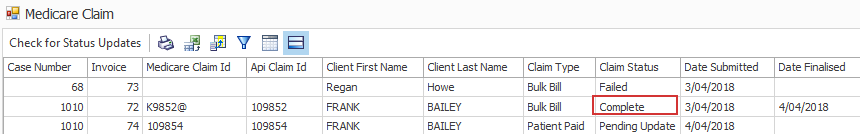
Completed claims
When a claim has been accepted by Medicare it is displayed in the Medicare claims report with Complete status. The date finalised and the payment amount is displayed.
Completed Medicare claim details are displayed at the case:
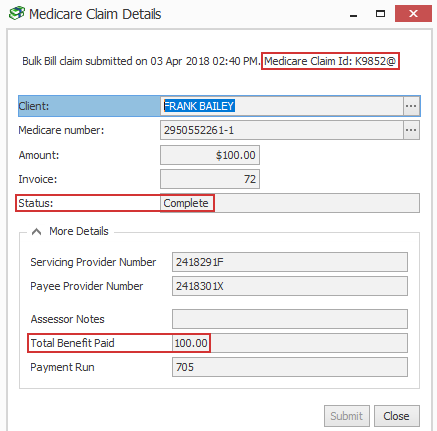
The Medicare Claim Id is displayed and the benefit paid.
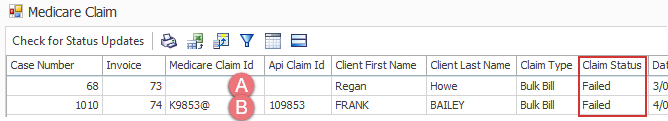
Failed claims
There are two ways claims can fail.
- When a claim fails at the first step of the process, i.e. validation by Case Manager, it is not submitted to Medicare.
- When a claim passes validation by Case Manager, is sent to Medicare and then rejected it is also reported with a Failed status.
It will be displayed in the Medicare claims report with a Failed status.
You can see that the Medicare Claim Id field is blank, indicating that it was never sent to Medicare.
This failed claim is not displayed at the invoice level because almost certainly the error(s) will be rectified and the claim will re-submitted.
However, in this situation the Medicare Claim Id is displayed and the Assessor Notes field will contain the error reason code number (see below) and any extra feedback received from Medicare.
These failed Medicare claims are displayed at the case.
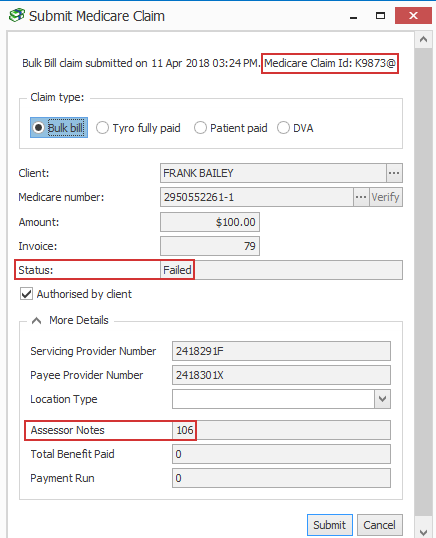
The Medicare Claim Id is displayed and the Assessor Notes field contains the error code and any additional notes returned.
In this situation it may be possible to address the issues that caused Medicare to reject the claim and then to submit a new claim.
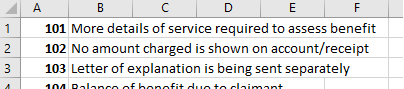
Medicare Error codes
The Medicare error codes are detailed at: https://www.humanservices.gov.au/organisations/health-professionals/enablers/medicare-digital-claiming-return-codes
This page also links to a downloadable spreadsheet listing all the 3 digit reason code numbers: