DVA claim life cycle
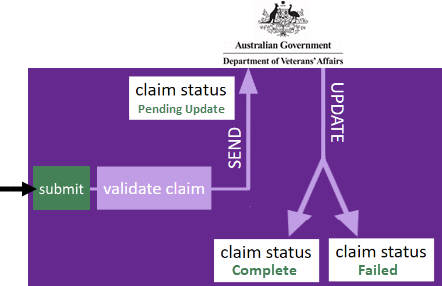
When you submit a DVA claim from an invoice it is first validated by Case Manager to ensure it contains the required information.
If it does not pass validation the problem(s) are displayed and the process goes no further. You should correct the claim details and re-submit the claim.
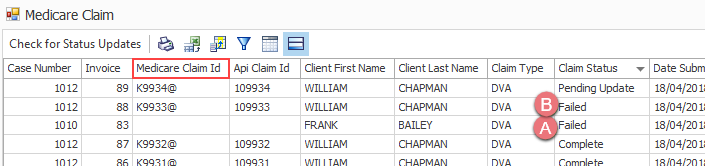
When the claim passes validation it is sent to DVA and given Pending Update status.
With time DVA either accepts and pays the claim or rejects it and give reason(s). Case Manager can monitor this process and when it has been finalised the claim outcome details are displayed. The claim is given a status of Complete or Failed as appropriate.
Pending claims are not updated automatically at Case Manager. You can check for updates any time to find out whether, when and how DVA has resolved them.
Note that you will see references to Medicare claims in screens when you manage your DVA claim. This is because the integrated claiming service provider is being used to process the claim.
Payment transactions
When DVA claims have been successfully completed you can create a payment transaction, as you would for any other direct deposit.
Claim status
A claim submitted to DVA has a status of Pending Update.
There are two possible outcomes:
- The claim is accepted and DVA pays the claim.
- The claim is rejected by DVA .
In Case Manager the claim will be given Complete status and the finalisation date, amount and payment run are displayed.
In Case Manager the claim will be given Failed status and the error code and any additional notes received from Medicare are displayed.
View claim details
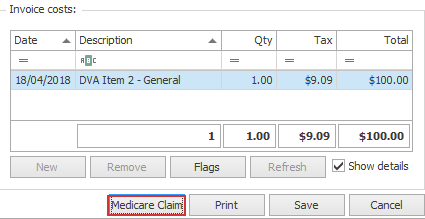
To view a claim select its invoice and click Medicare Claim, at the bottom of the invoice cost details:
Claim details are displayed including:
- the type of claim,
- the submission date,
- the claim Id
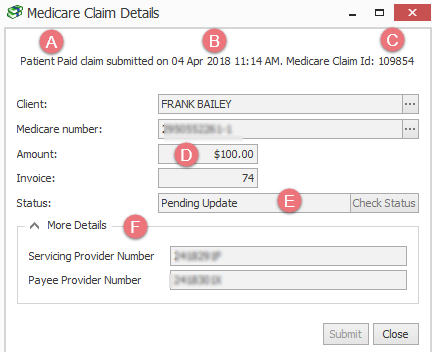
- the claim amount
- the claim status
- The More Details area contains further details, depending on the claim type.
- When the claim has been accepted by DVA you will also see the benefit paid and the payment run.
- When the claim has been rejected by DVA you will also see the error code and any extra feedback in the Assessor notes.
Check for updates to claims
Claims with Pending Update status are not updated automatically in Case Manager when DVA makes a decision to either accept or rejected them. Instead you need to request that Case Manager checks for any updates to pending claims.
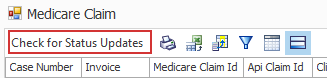
Multiple claims
To check for a updates to all claims with Pending Update status, click Check for Status Updates at the top of the Medicare claim grid:
You will need to close the current grid and re-open it again in order to refresh the list.
One claim
To check for an update to one claim locate the invoice, click Medicare Claim to view the claim details and click Check Status.
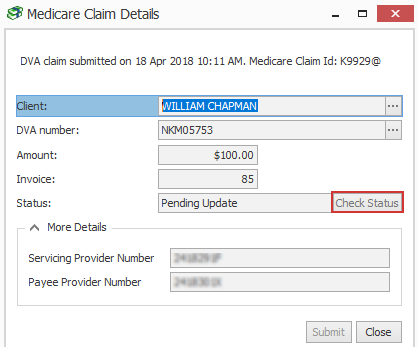
If there's been an update the claim status will change to Complete or Failed and the claim details are updated.
Completed claims
When a claim has been accepted by DVA it is displayed in the Medicare claims report with Complete status. The date finalised and the payment amount is displayed.
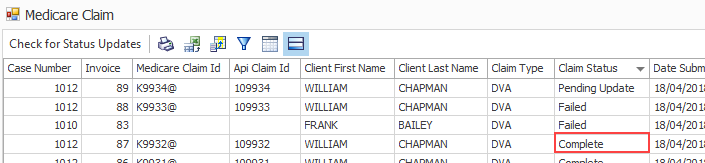
Completed DVA claim details are displayed at the case:
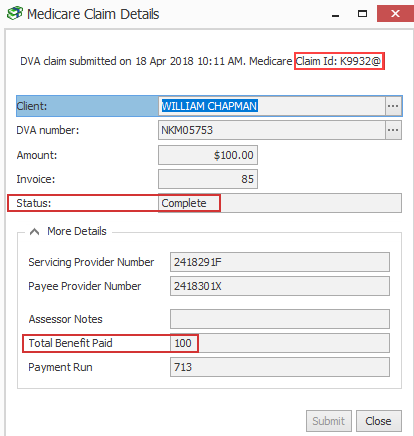
The Claim Id is displayed and the benefit paid.
Failed claims
There are two ways claims can fail.
- When a claim fails at the first step of the process, i.e. validation by Case Manager, it is not submitted to DVA.
- When a claim passes validation by Case Manager, is sent to DVA and then rejected it is also reported with a Failed status.
It will be displayed in the Medicare claims report with a Failed status.
You can see that the Claim Id field is blank, indicating that it was never sent to DVA.
This failed claim is not displayed at the invoice level because almost certainly the error(s) will be rectified and the claim will re-submitted.
However, in this situation the Claim Id is displayed and the Assessor Notes field will contain the error reason code number (see below) and any extra feedback received from Medicare.
These failed DVA claims are displayed at the case.
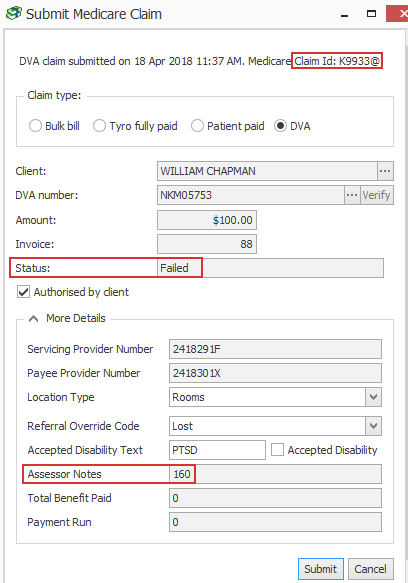
The Claim Id is displayed and the Assessor Notes field contains the error code and any additional notes returned.
In this situation it may be possible to address the issues that caused DVA to reject the claim and then to submit a new claim.
DVA error codes
A list of reason codes is at:
https://www.humanservices.gov.au/organisations/health-professionals/enablers/dva-reason-codes
These codes provide information on their assessment of a claim, such as why a claim has been rejected. The codes are accompanied by a brief explanation.