Medicare overview

Case Manager enables you to manage invoice payments from Medicare.
There are two Medicare options:
- Bulk Bill
- Patient paid
You claim the full invoice amount from Medicare.
When the claim is approved the money is paid into your bank account.
You accept full invoice payment from the patient and submit the patient's claim to Medicare.
When the claim is approved the money is paid to the patient.
Medicare claims are made from invoices. Case Manager monitors the status of these claims and the outcome, including when paid.
Case Manager utilises a claiming service provider to submit claims. There are additional charges to connect to this service. Please contact your sales team to discuss this charge.
All the other Medicare services are free, including validating and monitoring claims, and verifying cards.
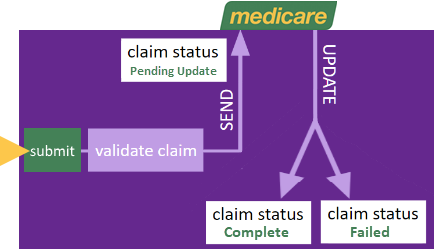
Claim life cycle
When you submit a claim from an invoice, the claim is validated to ensure it contains the required information. Then it is given a Pending Update status and sent to Medicare. Eventually, Medicare either accepts and pays the claim or rejects it and give reason(s). Case Manager monitors and reports on this process, recording the claim outcome details and giving the claim a status of Complete or Failed at the end of the process.
At any time you can check all pending claims in Case Manager to find out whether, when and how Medicare has resolved them. See Claim life cycle for more details.
Payment transactions
When Bulk Bill claims have been successfully completed you can create a payment transaction, as you would for any other direct deposit.
When the patient pays you would create a payment transaction on the spot, as you would for any other kind of payment.
Set up and requirements
Setting up this functionality is reasonably simple. Naturally you need to also make sure that Case Manager contains the information that Medicare requires so that this is included in your claims, see Setting up for Medicare.
Service types
The following service types are supported:
- S: Specialist
- O: General
- J: Allied
- K: Psych
The following are not supported:
- G: Dental
- L: Optical
- I: Speech Pathology
- P: Pathology services
- F: Community Nursing
DVA claims
The integrated claiming service provider also enables streamlined management of your DVA invoices. The process is similar to Medicare bulk billing, see DVA overview.